Do you know what causes altered mental status in sepsis? Brace yourself for a mind-blowing revelation.
This article will unveil the 6 common causes that lead to this perplexing condition. Prepare to have your understanding expanded as we explore:
– The inflammatory response
– Impaired brain perfusion
– Metabolic abnormalities
– Neurotoxic effects
– Blood-brain barrier dysfunction
– Neurological complications
Get ready to dive deep into the fascinating world of sepsis-induced altered mental status. Let’s unravel the mysteries together!
Table of Contents
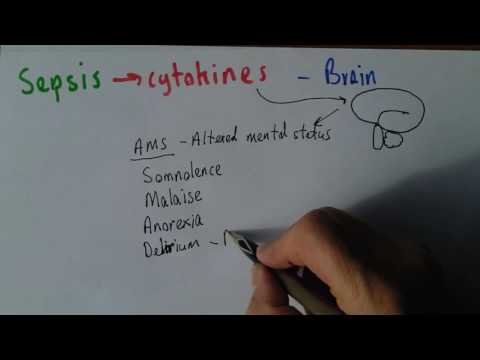
Related Video: "Sepsis 5, Brain and altered mental status" by Dr. John Campbell
Main Points
– Excessive cytokine release in sepsis can directly affect the blood-brain barrier, leading to neuroinflammation and disruption of normal brain function.
– Impaired brain perfusion and oxygenation can occur in sepsis, resulting in decreased blood flow, low blood pressure, and reduced oxygen levels in the brain, which can lead to neuronal injury and altered mental status.
– Fluid imbalance and electrolyte imbalances can occur in sepsis, leading to dehydration and disruptions in metabolic processes, which can further contribute to altered mental status.
– Microbial neurotoxins can directly damage brain cells and interfere with neurotransmitter signaling, leading to symptoms such as confusion, delirium, seizures, and coma in sepsis.
Inflammatory Response and Cytokine Release

You should understand that the inflammatory response and cytokine release play a crucial role in causing altered mental status in sepsis. When the body detects an infection, it initiates an immune response to fight off the invading pathogens. This response involves the activation of the immune system and the release of various inflammatory molecules known as cytokines. In sepsis, however, the immune response becomes dysregulated, leading to excessive and uncontrolled inflammation throughout the body.
The infection-induced inflammation triggers the release of pro-inflammatory cytokines such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha). These cytokines are essential for initiating the immune response and recruiting immune cells to the site of infection. However, in sepsis, the release of these cytokines becomes excessive, leading to a systemic inflammatory response that can have detrimental effects on the brain.
The inflammatory molecules can directly affect the blood-brain barrier, which normally protects the brain from harmful substances. The compromised blood-brain barrier allows the entry of cytokines and other inflammatory molecules into the brain, leading to neuroinflammation. This neuroinflammation can disrupt normal brain function and contribute to the development of altered mental status in sepsis.
In addition to the direct effects on the brain, the excessive cytokine release can also lead to systemic effects such as hypotension, which can further compromise brain function. The altered mental status in sepsis can range from confusion and agitation to delirium and coma, depending on the severity of the inflammatory response.
Impaired Brain Perfusion and Oxygenation
When blood flow to the brain is compromised and oxygen delivery is inadequate, it can lead to altered mental status in sepsis. Impaired cerebral circulation and hypoxemic brain injury are common causes of this condition. Here are some important points to consider:
– Decreased cerebral blood flow: In sepsis, the body’s response to infection can cause a decrease in blood flow to the brain. This can result from the dilation of blood vessels, which leads to low blood pressure and reduced perfusion to the brain.
– Hypoxia: Sepsis can also cause a decrease in oxygen levels in the blood, leading to hypoxia in the brain. This can occur due to impaired lung function, reduced oxygen-carrying capacity of the blood, or inadequate oxygen extraction by the tissues.
– Metabolic dysfunction: When the brain doesn’t receive enough oxygen and nutrients, it can lead to metabolic dysfunction. This can disrupt normal brain function and contribute to altered mental status in sepsis.
– Neuronal injury: Prolonged inadequate cerebral circulation and hypoxemia can result in neuronal injury, affecting the brain’s ability to process information and maintain normal mental function. This can manifest as confusion, disorientation, or even coma.
Understanding the impact of impaired brain perfusion and oxygenation in sepsis is crucial for early recognition and appropriate management of altered mental status in these patients.
Metabolic Abnormalities and Electrolyte Imbalances
Metabolic abnormalities and electrolyte imbalances can contribute to altered mental status in sepsis. Sepsis, a life-threatening condition caused by a systemic response to infection, can lead to fluid imbalances and organ dysfunction. These imbalances and dysfunctions can disrupt the normal functioning of the body, including the brain, resulting in changes in mental status.
Fluid imbalance, a common occurrence in sepsis, can have a significant impact on the body’s metabolic processes. In sepsis, there’s often an excessive loss of fluids due to increased capillary permeability and fluid leakage into surrounding tissues. This can lead to dehydration and electrolyte imbalances, such as hyponatremia (low sodium levels) and hypokalemia (low potassium levels). These imbalances can affect the brain’s ability to function properly and contribute to altered mental status.
Organ dysfunction, another consequence of sepsis, can also contribute to metabolic abnormalities and electrolyte imbalances. The dysfunction of organs like the liver and kidneys can disrupt the body’s ability to regulate electrolyte levels and metabolic processes. For example, liver dysfunction can impair the production of proteins involved in fluid balance, while kidney dysfunction can affect the excretion of waste products and electrolytes. These dysfunctions can further exacerbate the fluid imbalances and electrolyte disturbances in sepsis, leading to altered mental status.
Neurotoxic Effects of Microbial Toxins
Microbial toxins can disrupt normal brain function and contribute to altered mental status in sepsis. These neurotoxic effects can have serious consequences and require prompt recognition and treatment.
Here are some key points to consider:
– Mechanism and effects: Microbial neurotoxins, such as those produced by bacteria and viruses, can directly damage brain cells and interfere with neurotransmitter signaling. This disruption can lead to a range of neurological symptoms, including confusion, delirium, seizures, and coma. The severity of these effects can vary depending on the specific toxin and the individual’s immune response.
– Identification and diagnosis: Identifying the presence of microbial neurotoxicity can be challenging, as the symptoms can overlap with other causes of altered mental status in sepsis. However, a thorough evaluation of the patient’s clinical presentation, laboratory findings, and imaging studies can help guide the diagnosis. It’s important to consider microbial neurotoxicity as a potential cause, especially in patients with an unexplained decline in mental status.
– Treatment options: Treating microbial neurotoxicity involves addressing the underlying infection and providing supportive care to manage the neurological symptoms. This may include administering appropriate antibiotics or antiviral medications, controlling seizures with anticonvulsants, and maintaining cerebral perfusion and oxygenation. Timely treatment is crucial to minimize long-term neurological damage and improve patient outcomes.
– Future research: There’s ongoing research focused on understanding the mechanisms of microbial neurotoxicity and developing targeted therapies. Advances in this field may lead to more effective treatments and improved outcomes for patients with sepsis-related altered mental status.
Blood-Brain Barrier Dysfunction
Sometimes, sepsis can cause dysfunction in the blood-brain barrier, which can lead to altered mental status. The blood-brain barrier is a protective barrier that separates the brain from the bloodstream. It regulates the exchange of substances between the blood and the brain, allowing essential nutrients to enter while keeping harmful substances out. However, during sepsis, the blood-brain barrier can become disrupted, allowing harmful substances and immune cells to enter the brain.
When the blood-brain barrier is disrupted, it can lead to various complications, including brain edema. Brain edema is the accumulation of fluid in the brain tissue, which can increase pressure and cause damage to brain cells. This can result in altered mental status, including confusion, delirium, and even coma.
The exact mechanisms behind blood-brain barrier disruption in sepsis aren’t fully understood. However, it’s believed that the release of pro-inflammatory cytokines and other inflammatory mediators play a significant role. These inflammatory molecules can disrupt the tight junctions between the cells that make up the blood-brain barrier, allowing substances to leak into the brain.
Neurological Complications and Septic Encephalopathy
One possible neurological complication of sepsis is septic encephalopathy, which can result in altered mental status. Septic encephalopathy refers to a state of neurological dysfunction that occurs as a result of sepsis, a life-threatening condition caused by an infection. This condition is characterized by a wide range of cognitive impairments, including confusion, disorientation, and changes in attention and memory.
Here are four key points to understand about neurological complications and septic encephalopathy:
– Septic encephalopathy can occur in both adults and children who’ve sepsis.
– The exact mechanisms underlying septic encephalopathy aren’t fully understood, but it’s believed to involve an inflammatory response and the release of neurotoxic substances.
– The severity of neurological dysfunction can vary, ranging from mild confusion to profound coma.
– Early recognition and management of septic encephalopathy are crucial to prevent further neurological damage and improve patient outcomes.
It is important to note that septic encephalopathy is a serious condition that requires prompt medical attention. If you or someone you know is experiencing altered mental status in the context of sepsis, it’s important to seek immediate medical care to determine the underlying cause and initiate appropriate treatment.
Frequently Asked Questions
What Are the Specific Cytokines That Are Released During the Inflammatory Response in Sepsis?
During the inflammatory response in sepsis, specific cytokines are released. These cytokines play a role in the neuroinflammation that can lead to altered mental status.
How Does Impaired Brain Perfusion and Oxygenation Affect the Overall Outcome of Sepsis Patients?
Impaired brain perfusion and oxygenation in sepsis can have a significant impact on patient outcomes. Neurological complications, such as blood brain barrier dysfunction, can further worsen the overall condition of sepsis patients.
What Are the Most Common Metabolic Abnormalities and Electrolyte Imbalances Observed in Septic Patients?
Metabolic disturbances and electrolyte imbalances are common in septic patients. They can cause altered mental status, leading to confusion and disorientation. Proper management and treatment are crucial to prevent further complications.
Can You Provide Examples of Specific Microbial Toxins That Have Neurotoxic Effects in Sepsis?
In sepsis, specific microbial toxins like Clostridium difficile toxins and Staphylococcus aureus alpha toxin can have neurotoxic effects. These toxins contribute to altered mental status, which is a common cause of neurological changes in septic patients.


