Unlock the secrets of the mind as you delve into the depths of mental illness. In this enlightening article, we unveil the truth behind the seven potential causes of mental illness in the brain.
From genetic factors to childhood trauma, substance abuse to chronic stress, explore the intricate web of factors that contribute to these conditions.
Brace yourself for a journey through the complexities of the human brain, where truth awaits in every synaptic connection.
Table of Contents
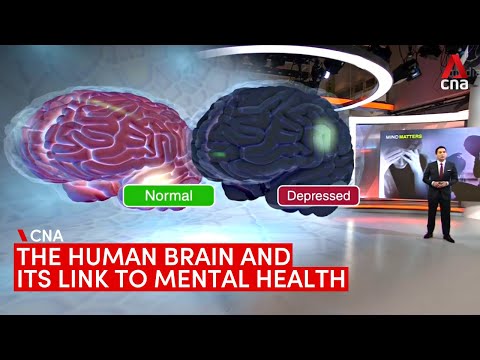
Related Video: "What causes mental illnesses? The human brain and its link to mental health" by CNA
Main Points
– Genetic factors play a crucial role in determining susceptibility to mental illnesses such as depression, anxiety, schizophrenia, and bipolar disorder.
– Neurochemical imbalances, influenced by genetic factors, contribute to the development of mental disorders. Disruptions in neurotransmitter production, release, or reuptake can lead to symptoms like depression, anxiety, and mood swings.
– Treatment options for mental illness include medications that regulate neurochemical imbalances, psychotherapy to manage emotions and develop healthier thought patterns, and lifestyle changes that support neurochemical balance.
– Environmental triggers, such as traumatic life events, chronic stress, and substance abuse, interact with genetic predisposition to influence the development of mental illnesses. Childhood trauma can have lasting effects on mental development, and chronic stress and inflammation can impair brain function and increase the risk of mental health disorders.
Genetic Factors

Your genetic makeup plays a significant role in determining your susceptibility to mental illnesses. Understanding the genetic factors behind mental illness is crucial in uncovering what causes mental illness in the brain, as well as how mental illness affects the brain. Numerous studies have shown that certain genes can increase the risk of developing mental disorders such as depression, anxiety, schizophrenia, and bipolar disorder.
Researchers have identified specific genes that are associated with an increased vulnerability to mental illness. For example, variations in the COMT gene have been linked to a higher risk of schizophrenia. This gene plays a role in regulating dopamine, a neurotransmitter involved in mood and cognition. Similarly, the serotonin transporter gene (SLC6A4) has been associated with an increased susceptibility to depression and anxiety disorders.
Genetic factors can influence how mental illness affects the brain. For instance, certain gene variations may affect the structure and function of brain regions involved in emotional regulation, memory processing, and decision-making. This can lead to alterations in neurotransmitter levels and disrupted neural circuits, contributing to the development and progression of mental disorders.
Neurochemical Imbalances
Neurochemical imbalances play a crucial role in the development of mental illness. These imbalances refer to disruptions in the levels or functioning of neurotransmitters in the brain.
Symptoms of mental illness such as depression, anxiety, and mood swings can be attributed to these imbalances.
Treatment options for neurochemical imbalances include medication to restore proper neurotransmitter levels and therapy to address underlying causes.
Additionally, research suggests a link between neurochemical imbalances and genetic factors, highlighting the complex interplay between biology and mental health.
Chemical Imbalances and Symptoms
When exploring the potential causes of mental illness in the brain, it is important to understand the impact of chemical imbalances and the symptoms they can manifest. Chemical imbalances in the brain, also known as neurochemical imbalances, occur when there is an abnormality in the levels of neurotransmitters or other chemicals that regulate brain function. These imbalances can lead to various mental health conditions such as depression, anxiety, and schizophrenia.
To help you better visualize the relationship between chemical imbalances and symptoms, here is a table outlining some common imbalances and the corresponding symptoms they may cause:
| Imbalance | Symptoms |
|---|---|
| Serotonin deficiency | Mood swings, depression, anxiety |
| Dopamine excess | Mania, hallucinations, delusions |
| GABA deficiency | Anxiety, restlessness, insomnia |
| Glutamate excess | Irritability, aggression, difficulty focusing |
Understanding these chemical imbalances and their associated symptoms is crucial for developing effective treatments and interventions for individuals with mental illness. By targeting these imbalances, healthcare professionals can help restore balance in the brain and alleviate symptoms, improving the overall well-being of those affected.
Treatment Options for Imbalances
To effectively address neurochemical imbalances and alleviate symptoms, healthcare professionals can offer various treatment options. These options are designed to restore the balance of neurotransmitters in the brain, thereby improving mental health.
Here are three treatment options that can be considered:
– Medication: Psychotropic medications, such as selective serotonin reuptake inhibitors (SSRIs) or mood stabilizers, can help regulate neurochemical imbalances. These medications work by targeting specific neurotransmitters and modulating their levels in the brain.
– Psychotherapy: Different forms of therapy, such as cognitive behavioral therapy (CBT) or dialectical behavior therapy (DBT), can be effective in treating neurochemical imbalances. Through these therapies, individuals can learn coping mechanisms, manage their emotions, and develop healthier thought patterns.
– Lifestyle changes: Making lifestyle modifications, such as exercising regularly, maintaining a balanced diet, and getting enough sleep, can also support neurochemical balance. Engaging in activities that promote relaxation and stress reduction, like meditation or yoga, can be beneficial as well.
Link Between Imbalances and Genetics
Understanding the genetic link to imbalances in the brain is crucial in uncovering the potential causes of mental illness.
Neurochemical imbalances, influenced by genetic factors, have been found to play a significant role in the development of mental disorders.
The brain relies on a delicate balance of neurotransmitters, such as serotonin, dopamine, and norepinephrine, to regulate mood, behavior, and cognition.
Genetic variations can disrupt the production, release, or reuptake of these neurotransmitters, leading to imbalances that contribute to mental illness.
For example, studies have identified specific gene mutations associated with conditions like depression, schizophrenia, and bipolar disorder.
Additionally, genes involved in the regulation of brain structure and function, such as synaptic plasticity and neurodevelopment, have also been implicated in mental disorders.
Environmental Triggers
The role of environmental triggers in the development of mental illness is a topic of great interest and ongoing research. Understanding the potential causes of mental illness in the brain requires a comprehensive examination of the various factors that can contribute to its manifestation.
Environmental triggers are external factors that can influence the development of mental illness in individuals who may be genetically predisposed. These triggers can interact with an individual’s genetic makeup and affect their brain chemistry and neural pathways.
Here are three key environmental triggers that have been associated with mental illness:
– Traumatic life events: Experiencing significant trauma, such as abuse, neglect, or a major life-changing event, can increase the risk of developing mental health disorders. Trauma can have long-lasting effects on the brain, leading to changes in mood, behavior, and cognitive function.
– Chronic stress: Prolonged exposure to high levels of stress can have detrimental effects on mental health. Stressful environments, such as a demanding work environment or ongoing interpersonal conflicts, can contribute to the development of anxiety disorders, depression, and other mental illnesses.
– Substance abuse: Substance abuse, including the use of drugs and alcohol, can have a profound impact on mental health. Substance abuse can alter brain chemistry, leading to the development of addiction and co-occurring mental health disorders.
It is important to note that environmental triggers alone aren’t sufficient to cause mental illness. The interplay between genetic factors and environmental triggers is complex and multifaceted. Further research is needed to better understand the specific mechanisms by which environmental triggers can contribute to the development of mental illness in susceptible individuals.
Childhood Trauma
Childhood trauma can have lasting effects on an individual’s mental health.
Research has shown that traumatic experiences in early childhood can disrupt normal brain development and increase the risk of developing mental illnesses later in life.
Understanding the impact of childhood trauma on the brain is crucial in order to develop effective interventions and support systems for those who’ve experienced such trauma.
Lasting Effects of Trauma
When experiencing lasting effects of trauma, it’s important to recognize how childhood trauma can significantly impact mental health. The effects of childhood trauma can be long-lasting and can manifest in various ways. Here are three key ways in which childhood trauma can affect mental health:
– Increased vulnerability to mental illness: Childhood trauma can increase the risk of developing mental illnesses such as depression, anxiety disorders, and post-traumatic stress disorder (PTSD). The traumatic experiences that occurred during childhood may disrupt the normal development of the brain, leading to persistent emotional and behavioral difficulties.
– Impaired social functioning: Children who’ve experienced trauma may struggle with forming and maintaining healthy relationships. They may have difficulties with trust, attachment, and emotional regulation, which can impact their ability to establish meaningful connections with others.
– Cognitive impairments: Childhood trauma can also affect cognitive functioning, including memory, attention, and problem-solving skills. The chronic stress associated with trauma can disrupt the development of the brain’s executive functions, leading to difficulties in academic performance and overall cognitive abilities.
Understanding the lasting effects of childhood trauma is crucial in order to provide appropriate support and interventions for individuals who’ve experienced such trauma. By acknowledging the impact of childhood trauma on mental health, we can work towards promoting healing and resilience in those affected.
Early Childhood Development
You may frequently underestimate the long-term impact of early childhood trauma on your mental development. Research has shown that traumatic experiences during this critical period can have lasting effects on the brain and contribute to the development of mental illness later in life.
Early childhood trauma, such as abuse, neglect, or witnessing violence, can disrupt the normal development of neural circuits involved in emotion regulation, memory processing, and stress response. This can lead to difficulties in regulating emotions, increased vulnerability to stress, and impaired cognitive function.
The effects of childhood trauma can persist into adulthood, shaping your mental health and well-being. Understanding the potential causes of mental illness, including the impact of early childhood trauma, is crucial for developing effective prevention and intervention strategies.
Substance Abuse
One potential cause of mental illness in the brain is substance abuse and its detrimental effects. Substance abuse refers to the excessive and harmful use of substances such as drugs and alcohol, which can lead to a range of mental health issues. Here are three key points to consider:
– Chemical imbalances: Substance abuse disrupts the delicate balance of neurotransmitters in the brain, which are responsible for regulating mood, emotions, and cognitive function. Prolonged substance abuse can result in alterations to the brain’s chemistry, leading to mental health disorders like depression, anxiety, and psychosis.
– Co-occurring disorders: Substance abuse often occurs alongside other mental illnesses. This phenomenon is known as a co-occurring disorder or dual diagnosis. Individuals with pre-existing mental health conditions may turn to substance abuse as a means of self-medication, exacerbating their symptoms and increasing the risk of developing further mental health issues.
– Structural changes: Chronic substance abuse can cause structural changes in the brain. Long-term drug or alcohol use can shrink brain volume, particularly in areas responsible for memory, decision-making, and emotional regulation. These structural changes can contribute to the development of mental illnesses, as well as impair cognitive functioning and behavior.
Understanding the link between substance abuse and mental illness is crucial for effective prevention and treatment strategies. By addressing substance abuse and its impact on the brain, we can strive towards better mental health outcomes and improved quality of life for individuals struggling with these challenges.
Chronic Stress
Continuing from the previous subtopic on substance abuse, chronic stress also plays a significant role in the potential causes of mental illness in the brain. Chronic stress refers to the prolonged exposure to stressful situations or events that can lead to negative psychological and physiological effects. When stress becomes chronic, it can disrupt the normal functioning of the brain and contribute to the development of mental health disorders.
To understand the impact of chronic stress on mental health, let’s examine some of the key ways in which it affects the brain:
| Brain Area | Effects of Chronic Stress |
| Prefrontal cortex | Impairs executive functions such as decision-making, problem-solving, and impulse control. |
| Hippocampus | Reduces neurogenesis, leading to memory and learning difficulties. |
| Amygdala | Increases amygdala activity, resulting in heightened emotional responses and an overactive stress response. |
| Hypothalamus | Activates the hypothalamic-pituitary-adrenal (HPA) axis, leading to the release of stress hormones like cortisol, which can disrupt the body’s natural balance. |
| Nucleus accumbens | Alters reward processing, contributing to anhedonia and a decreased ability to experience pleasure. |
As chronic stress continues to impact these brain areas, it can contribute to the development or exacerbation of mental illnesses such as anxiety disorders, depression, and post-traumatic stress disorder. Therefore, it is crucial to recognize and address chronic stress in order to promote mental well-being.
Inflammation and Immune System Dysfunction
Moving forward, let’s delve into the subtopic of ‘Inflammation and Immune System Dysfunction’ and explore its connection to the potential causes of mental illness in the brain.
– Inflammation: When the body detects an injury or infection, it initiates an immune response to protect itself. In some cases, this response can become chronic, leading to persistent inflammation. Studies suggest that chronic inflammation may contribute to the development of mental illnesses such as depression and anxiety.
– Immune System Dysfunction: The immune system plays a crucial role in defending the body against harmful pathogens. However, when the immune system is dysfunctional, it can lead to an imbalance in the body’s inflammatory response. This imbalance has been linked to various psychiatric disorders, including schizophrenia and bipolar disorder.
– Neuroinflammation: Inflammation in the brain, known as neuroinflammation, is a key factor in the development and progression of mental illnesses. It involves the activation of immune cells in the brain, called microglia, which release inflammatory molecules. These molecules can disrupt normal brain function and contribute to the manifestation of psychiatric symptoms.
Understanding the role of inflammation and immune system dysfunction in mental illness is essential for developing targeted treatments. By identifying and addressing these underlying factors, researchers hope to improve outcomes for individuals with mental health disorders.
Further research is needed to fully comprehend the complex relationship between inflammation, immune system dysfunction, and mental illness, but this area holds promise for future advancements in psychiatric care.
Frequently Asked Questions
Can Mental Illness Be Solely Attributed to Genetic Factors or Are There Other Contributing Factors?
Mental illness can't be solely blamed on genetics. Other factors also contribute. Environmental factors, such as trauma or stress, can play a role. It's important to consider the complex interplay between genes and the environment.
How Do Neurochemical Imbalances in the Brain Contribute to the Development of Mental Illness?
Neurochemical imbalances in the brain can play a significant role in the development of mental illness. Imbalances in neurotransmitters, such as serotonin or dopamine, can disrupt communication between brain cells, leading to symptoms of mental illness.
What Are Some Common Environmental Triggers That Can Lead to Mental Illness?
Some common environmental triggers that can lead to mental illness include chronic stress, traumatic experiences, substance abuse, social isolation, and unhealthy relationships. These factors can affect your brain chemistry and increase the risk of developing mental health disorders.


